
Jan 16 2023
- NEWS
Developing antibiotics that target multiple-drug-resistant bacteria
Researchers have designed and synthesized analogs of a new antibiotic that is effective against multidrug-resistant bacteria, opening a new front in the fight against these infections.
Antibiotics are vital drugs in the treatment of a number of bacterial diseases. However, due to continuing overuse and misuse, the number of bacteria strains that are resistant to multiple antibiotics is increasing, affecting millions of people worldwide. The development of new antibacterial compounds that target multiple drug resistant bacteria is also an active field of research so that this growing issue can be controlled.
A team led by Professor Satoshi Ichikawa at Hokkaido University has been working on the development of new antibacterials. Their most recent research, published in the journal Nature Communications, details the development of a highly effective antibacterial compound that is effective against the most common multidrug-resistant bacteria.
The team worked on a class of antibacterial compounds called sphaerimicins. These compounds block the function of a protein in the bacteria called MraY. MraY is essential for the replication of bacteria and plays a role in the synthesis of the bacterial cell wall; it is also not a target of currently available commercial antibiotics.
“Sphaerimicins are biological compounds, and have very complex structures,” explained Ichikawa, a corresponding author of the study. “We set out to design analogs to this molecule that would be easier to manufacture while also becoming more effective against MraY, thus increasing its antibacterial activity. The drug we designed was effective against methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococcus faecium (VRE), two of the more common multi-drug resistant bacteria.”
The team analysed structures of sphaerimicin A by molecular modelling assisted by calculation, and designed and synthesized two analogs of sphaerimicin, SPM1 and SPM2. These analogs were found to be effective against Gram positive bacteria.
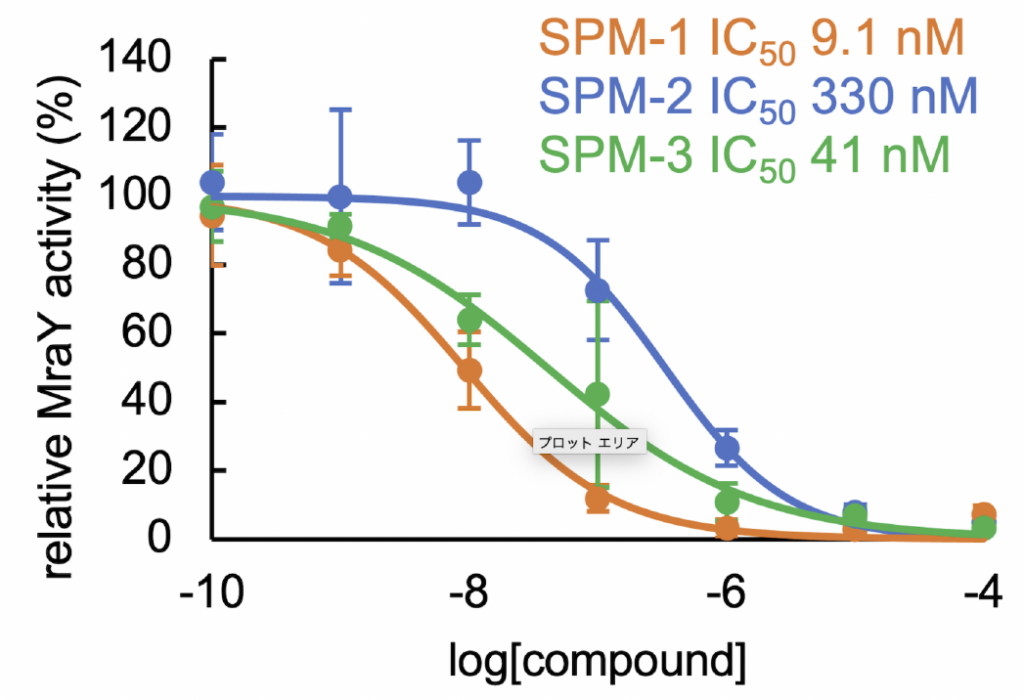
The sphaerimicin analogs (SPMs) inhibit the activity of MraY, and hence the replication of bacteria, with different degrees of effectiveness. The potency of the analog increases as the IC50 decreases (Takeshi Nakaya, et al. Nature Communications. December 20, 2022).
They then determined the structure of SPM1 bound to MraY. By studying this structure and comparing it to that of related antibacterial agents, they determined how to further simplify the molecules. They were successful in developing a simpler analog, SPM3, whose activity was similar to SPM1.
In addition to their effectiveness against MRSA and VRE, the SPMs were also effective against Mycobacterium tuberculosis, the bacteria that causes tuberculosis—and which has multidrug-resistant strains.
“Our most significant contribution is the construction of the core skeleton of sphaerimicin, which can be used to develop more antibacterial agents that target MraY and hence multidrug resistant strains. Sphaerimicin is most promising as MraY is also present in Gram negative bacteria,” Ichikawa concluded. Future work will include optimisation of the currently developed SPM molecules, and the development of sphaerimicin-containing antibiotic combinations to target a wider range of bacteria.
Original Article:
Takeshi Nakaya, et al. Synthesis of macrocyclic nucleoside antibacterials and their interactions with MraY. Nature Communications. December 20, 2022.
DOI: 10.1038/s41467-022-35227-z
Funding:
This research was supported in part by the Japan Society for the Promotion of Science (JSPS) KAKENHI Grant-in-Aid for Scientific Research (B) (JP16H05097, JP19H03345, JP21H03622), Grant-in Aid for Scientific Research on Innovative Areas “Frontier Research on Chemical Communications” (JP18H04599, 20H04757), JSPS KAKENHI Grant-in-Aid for Research for Young Scientist (JP19K16648), Takeda Foundation, The Tokyo Biomedical Research Foundation and was partly supported by Hokkaido University, Global Facility Center (GFC), Pharma Science Open Unit (PSOU), funded by MEXT under “Support Program for Implementation of New Equipment Sharing System”, Platform Project for Supporting Drug Discovery and Life Science Research (Basis for Supporting Innovative Drug Discovery and Life Science Research (BINDS)) from the Japan Agency for Medical Research and Development (AMED; JP18am0101093j0002, JP22ama121039, JP19ak0101118h0001, 21ak0101118h9903), Japan Science and Technology Agency (JST) START Program (ST211004JO), Japan Initiative for Global Research Network on Infectious Diseases (J-GRID) from the Ministry of Education, Culture, Sport, Science, and Technology in Japan, and MEXT for the Joint Research Program of the Research Center for Zoonosis Control, Hokkaido University, and National Institute of Health (R01GM120594). This work used NE-CAT beamlines (GM124165), a Pilatus detector (RR029205), an Eiger detector (OD021527) at the APS (DE-AC02-06CH11357).
Contacts:
Professor Satoshi Ichikawa
Center for Research and Education on Drug Discovery
Faculty of Pharmaceutical Sciences
Hokkaido University
Tel: +81-11-706-3228
Email: ichikawa[at]pharm.hokudai.ac.jp
Sohail Keegan Pinto (International Public Relations Specialist)
Public Relations Division
Hokkaido University
Tel: +81-11-706-2186
Email: en-press[at]general.hokudai.ac.jp




